Abstract
Objective: Vitamin D and iron are crucial micronutrients, particularly for children in phases of rapid growth and development, playing significant roles in bone and dental health, immune function, cognitive development, and energy metabolism. Despite the initiation of prophylaxis programs by the Turkish Ministry of Health, adherence and effectiveness remain variable, highlighting the need for localized research to evaluate these initiatives. This study aims to assess the prevalence and continuity of vitamin D and iron supplementation among families in Erzincan, and identify determinants influencing the sustainability of these practices.
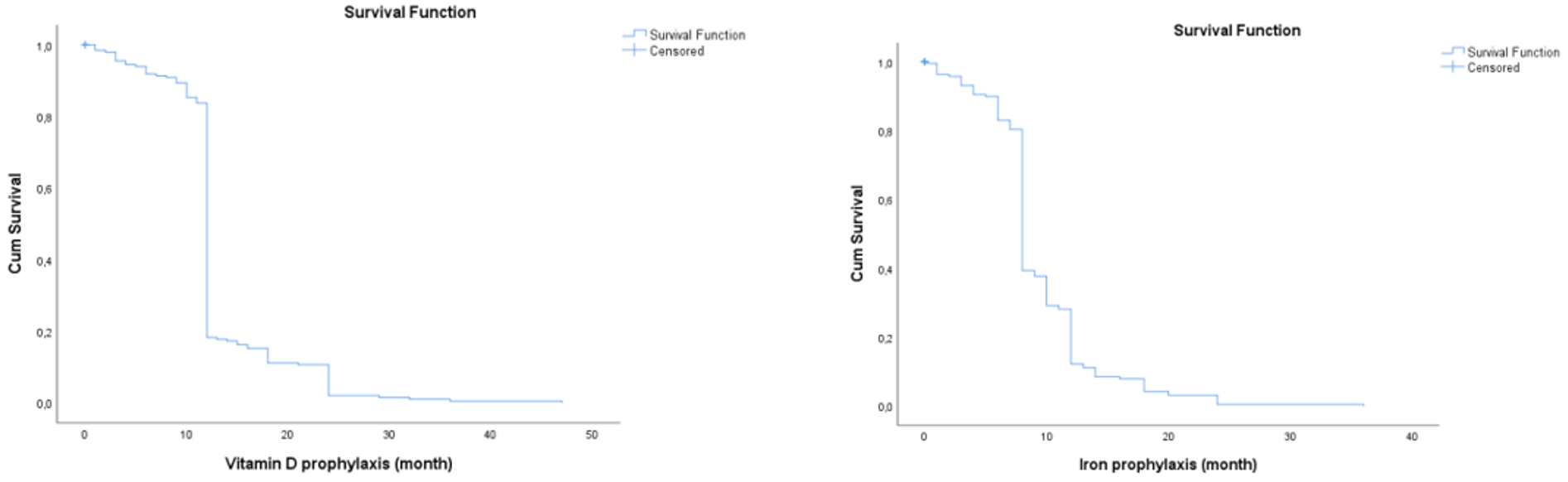
Methods: A cross-sectional and descriptive study was conducted among 200 families with children aged 1-5 years in the districts of Erzincan. Participants were recruited from family health centers using a convenience sampling method. Inclusion criteria encompassed families with children who met the age requirement, while exclusion criteria included children with special health conditions requiring high-dose supplementation. Data were collected through structured face-to-face questionnaires assessing supplementation practices, sources of medical advice, parental attitudes, and socio-demographic factors. Descriptive statistics summarized the data. The chi-square test and independent samples t-test assessed categorical and continuous variables, respectively. Multiple logistic regression identified factors influencing adherence, while Kaplan–Meier survival analysis evaluated supplementation duration.
Results: High rates of vitamin D (98.5%) and iron (94%) supplementation were observed, albeit with decreased adherence to the recommended durations (82.5% for vitamin D, 75.5% for iron). The absence of parental concern for their children’s health and concurrent use of another type of prophylaxis had a positive effect on prophylaxis use. A pediatrician recommended vitamin D and iron prophylaxis to 33% (n=66) of the participants, a family physician to 49% (n=98), and auxiliary health personnel to 3% (n=6) only, whereas 15% (n=32) were advised by more than one health professional. (p=0.008 for vitamin D prophylaxis; p=0.014 for iron prophylaxis). The multivariable logistic regression analyses revealed that parental concern about their infants’ health significantly impacted the continuity of vitamin D prophylaxis (p=0.010). However, demographic characteristics had no significant impact on supplementation practices.
Conclusion: Although vitamin D and iron supplementation rates are high in Erzincan, challenges in sustaining recommended durations suggest areas for improvement in prophylaxis programs. This study underscores the importance of healthcare professional recommendations and parental health perceptions in influencing supplementation practices. Recommendations include enhancing health education and accessibility to prophylaxis programs to improve sustainability and adherence.
Keywords: Vitamin D, iron, supplementation, child health, prophylaxis
Introduction
Vitamin D and iron are micronutrients of vital importance to human health. These nutrients play a critical role, especially in children who are in periods of rapid growth and development. Vitamin D is crucial for the regulation of bone and dental health, as well as the immune system, and it plays a significant role in the prevention of chronic diseases.[1,2] Iron, on the other hand, is essential for cognitive development, energy metabolism, and the transportation of oxygen, among other vital processes.[3,4] Nonetheless, inadequate intake of vitamin D and iron can lead to health issues such as childhood anemia and rickets. In this context, vitamin D and iron prophylaxis programs are considered a significant strategy for preventing such health problems.
The World Health Organization (WHO) and the United Nations Children’s Fund (UNICEF) recommend the development of national policies and the promotion of distribution efforts to prevent iron deficiency anemia and vitamin D deficiency.[5] These recommendations serve as a foundation for preventing vitamin D and iron deficiencies, particularly among high-risk groups.
In Türkiye, the Ministry of Health has initiated prophylaxis programs aimed at preventing vitamin D and iron deficiencies among children.[6] These programs are comprehensively designed to improve children’s health status and prevent nutritional deficiencies. However, the feasibility and effectiveness of these programs may vary due to a range of geographical and socioeconomic factors.
Despite the known benefits of vitamin D and iron supplementation, the literature on the effectiveness and adherence to prophylaxis programs in diverse regions remains scarce. This gap highlights the need for localized research to understand the dynamics affecting supplementation practices.
This study aimed to determine the prevalence and continuity of vitamin D and iron prophylaxis practices among families in a specific province and to identify factors affecting the sustainability of these practices. The findings of this research could contribute to the development of relevant health policies and prophylaxis programs, providing a significant reference for strategies aimed at preventing vitamin D and iron deficiencies.
Materials and Methods
This study was conducted using a cross-sectional and descriptive approach at family health centers located in the districts of Central, Kemah, and Tercan within the province of Erzincan.
Participant selection
Participants were selected from families living in the districts of Central, Kemah, and Tercan in Erzincan province, who had children aged between 1 to 5 years. The individuals selected for this study were those with the cognitive capacity to understand and respond to the research questions. Therefore, the target population segment for this study comprises families that match the specified geographical and demographic characteristics.
Babies with a history of premature birth (<36 weeks) and those receiving treatment doses of vitamin D or iron supplementation because of certain health conditions were excluded from the study. The exclusion criteria also included those requiring high doses of vitamins or minerals because of conditions such as rickets, osteomalacia, or malabsorption. This measure ensures the validity and reliability of the research findings for the general population, unaffected by special health conditions requiring treatment.
Method
This study focused on the iron and vitamin D prophylaxis programs initiated by the Ministry of Health in the years 2004 and 2005. A questionnaire was administered to parents, covering topics such as the status and duration of their children’s use of iron and vitamin D, reasons for discontinuation, the preparations used, and who initiated the prophylaxis. Demographic information was also collected.
Preliminary permission for this study was obtained from the Erzincan Provincial Health Directorate. The following approval from the Erzincan University Clinical Research Ethics Committee with the number 2023-16/10, the study was commenced. Participation in the study was voluntary, and oral and written consent was obtained from all participants. No fee was paid for participation.
The questionnaire was administered to all participants who agreed to participate and met the participation criteria, without randomization. Although the exact population numbers for different age groups are not specified, according to 2022 data from the Turkish Statistical Institute (TUIK), the population under the age of 4 years in Erzincan province is 13.688. Considering the population growth rate, it is estimated that there are approximately 16,000 children under the age of 5 in Erzincan province in 2023. In a study by Karapınar et al., the rate of iron prophylaxis usage in infants older than 1 month was 80.5%.[7] Using a 90% confidence interval and a 5% significance level, the sample size was determined to be a minimum of 169 according to the formula
n=[DEFF × N × Z² × p(1–p)] / [d² × (N–1) + Z² × p(1–p)]. In this context, interviews were conducted with 200 individuals.
In accordance with Türkiye’s health policies, individuals who received vitamin D prophylaxis for at least twelve months and iron prophylaxis for at least eight months were considered to have received adequate prophylaxis.
Statistical analysis
The data were analyzed using the IBM SPSS 25.0 software package (SPSS Inc., Chicago, IL, USA). The assumption of normal distribution was assessed using the Kolmogorov –Smirnov test, and the homogeneity of variances was evaluated using the Levene test. The descriptive statistics of the data were given as mean±standard deviation, frequency (percentage) for continuous and categorical variables, respectively. Chi- square, Fisher’s exact test, Mann –Whitney U test, and Independent samples t-test were used to evaluate differences between groups. Multiple logistic regression analysis was used to identify the factors affecting the continuity of prophylaxis application. Variables with p-values less than 0.20 in univariate analyses were selected as candidate variables for the multiple model. The multiple logistic regression model was initially constructed using the Forward (LR) method, and clinically significant variables were then added to the final model using the Enter method, and odds ratios were adjusted. The mean duration of Vitamin D and Iron prophylaxis was analyzed using the Kaplan-Meier test.
A statistical significance level of p<0.05 was accepted.
Results
A total of 200 parents and their children were included in the study. The average age of the children was 34.34 months (min=12, max=60). The average age of the mothers was 31.74±4.94, while the average age of the fathers was 34.40±6.14. Of the participants, 42% (n=84) had one child, and 37.5% (n=75) had two children. The highest number of children owned was five, accounting for 1% (n=2) of the participants. Other demographic data of the participants are provided in Table 1.
| Table 1. The demographic data of the participants | ||
|
|
|
|
| Infant Gender | ||
| Male |
|
|
| Female |
|
|
| Mother's Employment Status | ||
| Full-time employed |
|
|
| Part-time employed |
|
|
| Not employed |
|
|
| Father's Employment Status | ||
| Full-time employed |
|
|
| Part-time employed |
|
|
| Not employed |
|
|
| Mother's Education Level | ||
| Illiterate/Primary Education |
|
|
| High School |
|
|
| University and above |
|
|
| Father’s Education Level | ||
| Illiterate/Primary Education |
|
|
| High School |
|
|
| University and Above |
|
|
| Number of Children | ||
| One |
|
|
| Two or more |
|
|
At least one month of vitamin D supplementation was received by 98.5% (n=197) of the children, and 94% (n=188) received iron prophylaxis. The rate of taking vitamin D for the recommended duration of 12 months dropped to 82.5% (n=165), whereas the rate of taking iron for 8 months was 75.5% (n=151). Data related to the participants’ vitamin D and iron prophylaxis status are presented in Table 2.
| Table 2. Participants’ status on receiving vitamin D and iron prophylaxis | ||
|
|
|
|
| Receiving Vitamin D Prophylaxis | ||
| Yes |
|
|
| No |
|
|
| Receiving Vitamin D Prophylaxis for an Adequate Duration | ||
| Yes |
|
|
| No |
|
|
| Frequency of Vitamin D Intake | ||
| Daily |
|
|
| Other |
|
|
| Form of Vitamin D | ||
| Drops |
|
|
| Other |
|
|
| Receiving Iron Prophylaxis | ||
| Yes |
|
|
| No |
|
|
| Receiving Iron Prophylaxis for an Adequate Duration | ||
| Yes |
|
|
| No |
|
|
| Frequency of Iron Intake | ||
| Daily |
|
|
| Other |
|
|
| Form of Iron | ||
| Drops |
|
|
| Other |
|
|
| Reason for Not Receiving Prophylaxis | ||
| Not recommended |
|
|
| Adverse effects |
|
|
| Other |
|
|
A pediatrician recommended vitamin D and iron prophylaxis to 33% (n=66) of the participants, a family physician to 49% (n=98), and auxiliary health personnel to 3% (n=6) only, whereas 15% (n=32) were advised by more than one health professional (p=0.008 for vitamin D prophylaxis; p=0.014 for iron prophylaxis). The status of vitamin D and iron prophylaxis intake and associated factors are presented in Table 3 and Table 4, respectively.
| * Fisher exact test | |||||||
| Table 3. Status of infants receiving vitamin D prophylaxis | |||||||
|
|
|||||||
|
|
|
||||||
|
|
|
|
|
|
|
|
|
| Mother’s Employment Status | |||||||
| Full-time employed |
|
|
|
|
|
|
|
| Part-time employed |
|
|
|
|
|||
| Not employed |
|
|
|
|
|||
| Mother’s Education Level | |||||||
| Illiterate/Primary Education |
|
|
|
|
|
|
|
| High School |
|
|
|
|
|||
| University and above |
|
|
|
|
|||
| Father’s Employment Status | |||||||
| Full-time employed |
|
|
|
|
|
|
|
| Part-time employed |
|
|
|
|
|||
| Not employed |
|
|
|
|
|||
| Father’s Education Level | |||||||
| Illiterate/Primary Education |
|
|
|
|
|
|
|
| High School |
|
|
|
|
|||
| University and above |
|
|
|
|
|||
| Infant Gender | |||||||
| Male |
|
|
|
|
|
|
|
| Female |
|
|
|
|
|||
| Number of Children | |||||||
| One |
|
|
|
|
|
|
|
| Two or more |
|
|
|
|
|||
| Administering Iron Supplements to Infants | |||||||
| Yes |
|
|
|
|
|
||
| No |
|
|
|
|
|||
| Concern About Infants’ Health | |||||||
| Yes |
|
|
|
|
|
|
|
| No |
|
|
|
|
|||
| *Fisher exact test | |||||||
| Table 4. Status of infants receiving iron prophylaxis | |||||||
|
|
|||||||
|
|
|
||||||
|
|
|
|
|
|
|
|
|
| Mother’s Employment Status | |||||||
| Full-time employed |
|
|
|
|
|
|
|
| Part-time employed |
|
|
|
|
|||
| Not employed |
|
|
|
|
|||
| Mother’s Education Level | |||||||
| Illiterate/Primary Education |
|
|
|
|
|
|
|
| High School |
|
|
|
|
|||
| University and above |
|
|
|
|
|||
| Father’s Employment Status | |||||||
| Full-time employed |
|
|
|
|
|
|
|
| Part-time employed |
|
|
|
|
|||
| Not employed |
|
|
|
|
|||
| Father’s Education Level | |||||||
| Illiterate/Primary Education |
|
|
|
|
|
|
|
| High School |
|
|
|
|
|||
| University and above |
|
|
|
|
|||
| Infant Gender | |||||||
| Male |
|
|
|
|
|
|
|
| Female |
|
|
|
|
|||
| Number of Children | |||||||
| One |
|
|
|
|
|
|
|
| Two or more |
|
|
|
|
|||
| Administering a Vitamin D Supplement to an Infant | |||||||
| Yes |
|
|
|
|
|
||
| No |
|
|
|
|
|||
| Concern About Infants’ Health | |||||||
| Yes |
|
|
|
|
|
|
|
| No |
|
|
|
|
|||
The multivariable logistic regression analyses revealed that parental concern about their infants’ health significantly impacted the continuity of vitamin D prophylaxis (p=0.010). Specifically, children whose parents expressed concern about their health were more likely to adhere to the recommended supplementation duration (Table 5).
| Table 5. Results of multivariable logistic regression analysis for vitamin D and iron prophylaxis | ||||||
|
|
||||||
| Vitamin D |
|
|
|
|
|
|
| Mother’s Education Level |
|
|||||
| Illiterate/Primary Education |
|
|||||
| High School |
|
|
|
|
|
|
| University and above |
|
|
|
|
|
|
| Number of Children |
|
|||||
| One |
|
|||||
| Two or more |
|
|
|
|
|
|
| Concern About Infants’ Health |
|
|||||
| Yes |
|
|||||
| No |
|
|
|
|
|
|
|
|
||||||
| Iron |
|
|
|
|
|
|
| Mother’s Education Level |
|
|||||
| Illiterate/Primary Education |
|
|||||
| High School |
|
|
|
|
|
|
| University and above |
|
|
|
|
|
|
| Number of Children |
|
|||||
| One |
|
|||||
| Two or more |
|
|
|
|
|
|
| Concern About Infants’ Health | ||||||
| Yes |
|
|
||||
| No |
|
|
|
|
|
|
As shown in the Kaplan–Meier survival curve, the average duration of vitamin D prophylaxis intake was 13.025±0.409 months, whereas the average iron prophylaxis intake duration was 9.471±0.344 months (Figure 1).
Discussion
This study examined the status, prevalence, and associated factors of vitamin D and iron prophylaxis intake in the Erzincan province. These findings indicate high levels of vitamin D and iron supplementation. However, the decrease in the proportion of children receiving prophylaxis for the recommended duration suggests some challenges in the sustainability of these programs.
After the “Iron-like Turkey” campaign, a study conducted to assess the situation found that 68.8% of 1589 children received iron prophylaxis.[8] Similar rates have been observed in other national studies as well.[7,9] In a study conducted with 1002 children in İzmir, Türkiye, it was observed that 77% of the children received vitamin D prophylaxis, whereas the rates of adherence for the recommended duration dropped to 57%.[10] These findings indicate that iron and vitamin D prophylaxis are widely adopted across Türkiye; however, the effectiveness of these programs may be limited due to low adherence rates for the recommended durations. In a global context, similar adherence issues have been reported. A study in the United Kingdom highlighted that despite high initial compliance with vitamin D supplementation programs, adherence to recommended durations declined significantly due to lack of parental awareness and inconsistent follow-up by healthcare providers.[11] Similarly, a study in Canada found that while 80% of infants were initially given vitamin D supplementation, only about half continued for the recommended duration, with parental forgetfulness and misconceptions about dietary sufficiency being major barriers.[12] This situation underscores the need for further research on the feasibility and sustainability of prophylaxis programs. Moreover, enhancing awareness and education programs within target groups to increase and sustain the intake of these supplements is crucial.
Iron and vitamin D play a critical role in the growth and development of children, and deficiencies can lead to various health issues. The concurrent implementation of iron and vitamin D prophylaxis can create synergistic effects on child health; hence, prophylaxis programs often address these two essential micronutrients comprehensively.[13,14] Our study revealed a tendency for children receiving iron prophylaxis to also receive vitamin D prophylaxis, and vice versa. This correlation has been observed in other studies as well. A recent systematic review on micronutrient supplementation found that integrating vitamin D and iron supplementation into a single public health program increased overall adherence and effectiveness.[15] Similarly, a study conducted in Nepal found that children who adhered to iron and zinc supplementation were also more likely to adhere to vitamin A supplementation, suggesting that once parents commit to one prophylaxis measure, they are more likely to adopt others as well.[16] This relationship could be attributed to increased access to healthcare services and health awareness. The adoption of one recommendation by health professionals is likely to lead to the acceptance of another. These findings underline the necessity of an integrated approach to iron and vitamin D prophylaxis, offering a scientific basis for the development of related health policies and intervention programs.
Our research suggests that parents without concerns about their child’s health may be more inclined to use iron and vitamin D prophylaxis. This could stem from a strong belief among parents regarding the benefits of prophylaxis practices for supporting their children’s healthy growth and development. In other words, parents might view the use of prophylaxis as an indicator of their children’s existing health, thereby harboring fewer health-related concerns. A study in Germany found similar behavioral patterns among parents, where those with higher health literacy were more likely to adhere to micronutrient supplementation guidelines for their children.[17] This finding aligns with existing literature suggesting that parental beliefs, health literacy, and trust in medical guidance are critical determinants of adherence to micronutrient supplementation in children.[18] This finding reflects general confidence in the efficacy of prophylaxis programs and could signify proactive behaviors by parents in maintaining child health.[19]
Although our study did not find statistically significant associations between socio-demographic factors and adherence to vitamin D and iron supplementation, existing literature suggests that certain barriers may still negatively influence prophylaxis practices. For instance, adverse effects such as gastrointestinal discomfort are commonly reported reasons for early discontinuation of iron supplements in other studies.[20] Furthermore, inadequate counseling, inconsistent follow-up, and limited understanding of the long-term benefits of supplementation have been associated with poor adherence in various contexts.[11] While these factors did not reach significance in our cohort, they remain critical considerations, particularly in settings with lower health literacy or limited healthcare access. Therefore, continued efforts to address these potential barriers—through clearer communication, follow-up systems, and parent-targeted education—may help enhance the effectiveness of national supplementation programs. Consequently, health professionals and policymakers should develop strategies that reduce parental health concerns and encourage participation in prophylaxis programs. Integrating digital health solutions, such as mHealth apps and SMS reminders, telehealth programs, AI-driven digital platforms can enhance adherence to prophylaxis programs by providing real-time supplementation reminders, educational content, and direct communication with healthcare providers.[11,17,19]
Limitations of the Study
Acknowledging the limitations of our study and interpreting the findings considering these limitations are crucial. For instance, because of the cross-sectional design of the study, it is not possible to draw definitive conclusions about cause– effect relationships. Furthermore, relying on self-reported data from participants introduces the potential for reporting bias and recall errors. Therefore, caution should be exercised when extrapolating our findings to the general population.
Conclusion
This study examined the status, prevalence, and associated factors of vitamin D and iron prophylaxis intake in the Erzincan province. The findings demonstrate that demographic characteristics (such as the educational level of parents, employment status, number of children, and infant gender) do not significantly influence vitamin D and iron prophylaxis intake. Moreover, the high rates of vitamin D and iron prophylaxis intake reflect the success of health policies and childhood prophylaxis programs in Türkiye. However, the low rates of adherence to the recommended durations highlight the potential challenges in the sustainability and continuity of these programs. Considering this study’s findings, various recommendations can be made for more effective planning and implementation of health policies and prophylaxis programs. Health education and awareness campaigns could help increase participation rates by providing parents with more information on the importance of prophylaxis programs. Additionally, developing strategies to enhance the feasibility and accessibility of prophylaxis programs could play a critical role in ensuring program continuity.
Ethical approval
This study has been approved by the Erzincan Binali Yıldırım University Clinical Research Ethics Committee (approval date 21.09.2023, number 2023-16/10). Written informed consent was obtained from the participants.
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Amrein K, Scherkl M, Hoffmann M, et al. Vitamin D deficiency 2.0: an update on the current status worldwide. Eur J Clin Nutr. 2020;74:1498-1513. https://doi.org/10.1038/s41430-020-0558-y
- Cashman KD. Vitamin D deficiency: defining, prevalence, causes, and strategies of addressing. Calcif Tissue Int. 2020;106:14-29. https://doi.org/10.1007/s00223-019-00559-4
- Lozoff B, Georgieff MK. Iron deficiency and brain development. Semin Pediatr Neurol. 2006;13:158-65. https://doi.org/10.1016/j.spen.2006.08.004
- Pasricha SR, Tye-Din J, Muckenthaler MU, Swinkels DW. Iron deficiency. Lancet. 2021;397:233-248. https://doi.org/10.1016/S0140-6736(20)32594-0
- World Health Organization (WHO), UNICEF. Global strategy for infant and young child feeding. Geneva: WHO; 2003. Available at: https://www.who.int/publications/i/item/9241562218
- Hatun Ş, Ozkan B, Bereket A. Vitamin D deficiency and prevention: Turkish experience. Acta Paediatr. 2011;100:1195-9. https://doi.org/10.1111/j.1651-2227.2011.02383.x
- Karapınar TH, Bildik O, Köker SA, et al. The evaluation of taking iron supplements in children aged 6 months-2 years. The Journal of Pediatric Research. 2017;4:156-159. https://doi.org/10.4274/jpr.37790
- Yalçın SS, Tezel B, Yurdakök K, et al. A community-based iron supplementation program, “Iron-Like Turkey”, and the following prevalence of anemia among infants aged 12-23 months. Turk J Pediatr. 2013;55:16-28.
- Çullas-İlarslan NE, Günay F, İleri DT, Elhan AH, Ertem M, Arsan S. Investigation of the frequency of iron insufficiency among infants in a population in which routine iron supplementation is implemented. Turk J Pediatr. 2018;60:22-31. https://doi.org/10.24953/turkjped.2018.01.004
- Koc F, Halicioglu O, Sutcuoglu S, Asik Akman S, Aksit S. Vitamin D supplementation during the first two years of life in Izmir, Turkey. Minerva Pediatr. 2014;66:141-146.
- Moon RJ, Davies JH, Cooper C, Harvey NC. Vitamin D, and maternal and child health. Calcif Tissue Int. 2020;106:30-46. https://doi.org/10.1007/s00223-019-00560-x
- Gallo S, Jean-Philippe S, Rodd C, Weiler HA. Vitamin D supplementation of Canadian infants: practices of Montreal mothers. Appl Physiol Nutr Metab. 2010;35:303-309. https://doi.org/10.1139/H10-021
- Grindulis H, Scott PH, Belton NR, Wharton BA. Combined deficiency of iron and vitamin D in Asian toddlers. Arch Dis Child. 1986;61:843-848. https://doi.org/10.1136/adc.61.9.843
- Kan A, Sayli T. Effects of vitamin D prophylaxis on oral iron treatments of iron deficiency anemia. Minerva Pediatr (Torino). 2022;74:761-765. https://doi.org/10.23736/S2724-5276.20.06073-9
- Prentice A, Schoenmakers I, Jones KS, Jarjou LMA, Goldberg GR. Vitamin D deficiency and its health consequences in Africa. Clin Rev Bone Miner Metab. 2009;7:94-106. https://doi.org/10.1007/s12018-009-9038-6
- Freitas BACD, Lima LM, Moreira MEL, et al. Micronutrient supplementation adherence and influence on the prevalences of anemia and iron, zinc and vitamin A deficiencies in preemies with a corrected age of six months. Clinics (Sao Paulo). 2016;71:440-8. https://doi.org/10.6061/clinics/2016(08)06
- Schwarzenberg SJ, Georgieff MK, COMMITTEE ON NUTRITION. Advocacy for improving nutrition in the first 1000 days to support childhood development and adult health. Pediatrics. 2018;141:e20173716. https://doi.org/10.1542/peds.2017-3716
- Hoffmann MR, Alzaben AS, Enns SE, Marcon MA, Turner J, Mager DR. Parental health beliefs, socio-demographics, and healthcare recommendations influence micronutrient supplementation in youth with celiac disease. Can J Diet Pract Res. 2016;77:47-53. https://doi.org/10.3148/cjdpr-2015-035
- Beatton T, Moores CJ, Sarkar D, Sarkar J, Silva Goncalves J, Vidgen HA. Do parental preferences predict engagement in child health programs? Health Econ. 2021;30:2686-2700. https://doi.org/10.1002/hec.4402
- Tosyali M, Koç F. Adherence to iron supplementation during the first year of life infants in Izmir, Turkey. Medicine (Baltimore). 2024;103:e38926. https://doi.org/10.1097/MD.0000000000038926
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.