Abstract
Objective: Hypertension is an important health problem that affects the entire population and causes mortality and morbidity. Although there are screening recommendations in different diagnosis and treatment guidelines, there are studies showing that blood pressure measurement is skipped during examination in practice. This study aimed to evaluate the blood pressure measurement status in adults applying to different outpatient clinics in our hospital.
Methods: In our cross-sectional-analytical study, the data of patients who applied to the Karadeniz Technical University Farabi Hospital polyclinics for any reason between 01.01.2023 and 01.01.2024 were scanned retrospectively from the hospital information system. Patients who were over 18 years of age with their anamnesis taken and physical examination information completed were included in the study. Patients selected by random sampling method from 24 different branch clinics were included in the study. A sample of 215 people was calculated from each of the clinics. Patients’ age, gender, chronic disease status, medication use information, and blood pressure measurement data were collected.
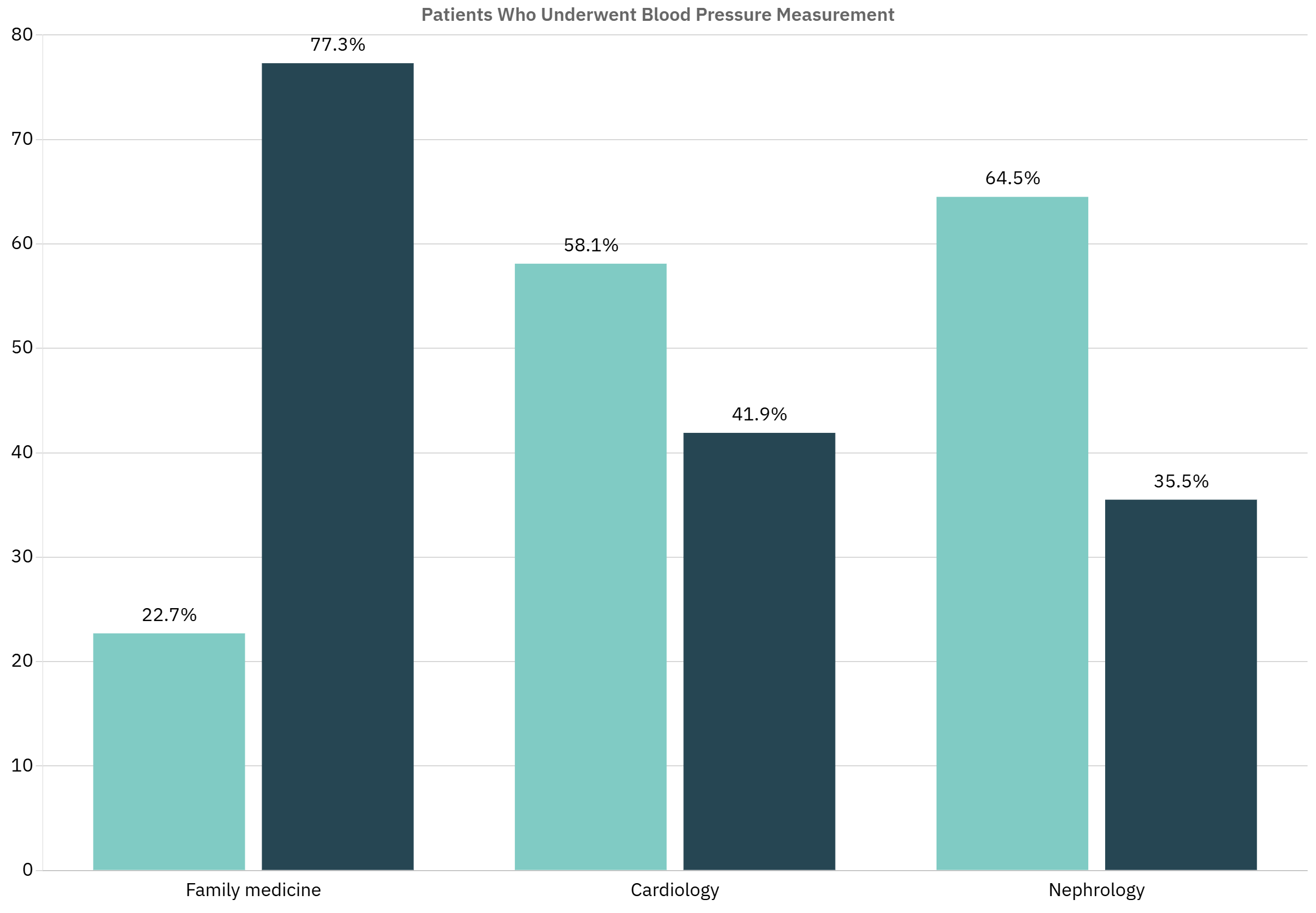
Results: The median age of the 5160 participants was 48 (IQR: 32-62) years. 58.4% (n=3015) of the participants were women. 13.8% of the participants had their blood pressure measured during their outpatient clinic examination. While the departments that performed the most measurements were nephrology, cardiology and general internal medicine, it was observed that none of the patients had their blood pressure measured in ten outpatient clinics, including oncology and neurosurgery. 49.7% (n=354) of the individuals whose blood pressure was measured already had hypertension diagnosis. When blood pressure staging was done according to the blood pressure measurement results, 46.1% (n=328) had increased blood pressure. 77.3% of individuals whose blood pressure was measured in the family practice outpatient clinic did not have a predetermined hypertension diagnosis.
Conclusion: The results reveal that the rate of blood pressure measurement, which is a part of the physical examination in outpatient clinics, is much lower than it should be. In order to ensure early diagnosis and blood pressure control of a chronic disease such as hypertension, which is common in society and can have serious complications, every polyclinic visit of the patients should be considered as an opportunity to measure blood pressure.
Keywords: Blood pressure, hypertension, blood pressure determination, screening, family practice
Introduction
Hypertension is defined as a condition where systolic blood pressure (SBP) is ≥ 140 mmHg and/or diastolic blood pressure (DBP) is ≥ 90 mmHg based on repeated clinic blood pressure measurements, according to the European Society of Cardiology (ESC/ESH) and many other guidelines.[1-4] Hypertension is a significant chronic disease affecting the entire population, associated with multifactorial problems, and poses a substantial burden on health and economics.[4] The global economic burden of high blood pressure is estimated to be approximately $370 billion, accounting for about 10% of global health expenditures.[5] The Global Burden of Disease analysis in 2017 identified high systolic blood pressure as the cause of death for 10.4 million individuals.[6] According to the Turkish Statistical Institute (TURKSTAT) evaluation of mortality statistics for 2022, deaths due to circulatory system diseases ranked first at 35.4%, with hypertension-related deaths constituting 9.9% of circulatory system deaths.[7] The PURE (Prospective Urban Rural Epidemiology) study conducted in 17 countries across five continents showed a prevalence of hypertension of 40.8%, particularly rising to 53.3% among individuals over 50 years of age. It was found that 46.5% of participants with hypertension were aware of their diagnosis, with 87.5% of those aware receiving pharmacological treatment, and only 32.5% of those treated having their blood pressure under control.[8] In Türkiye, the PatenT2 study conducted in 2012 found a hypertension prevalence of 30.3%[9], while the TURDEP-II study conducted in 2013 reported a prevalence of 31.4%.[10] The PURE Turkey study reported a prevalence of hypertension at 41.1%.[11] According to the PatenT2 study, awareness of hypertension in Türkiye was 54%, the proportion of those receiving treatment was 47.4%, and the proportion of those with controlled blood pressure was 28.7%.[9]
A study published in 2022 indicated that the average number of annual examinations performed in secondary and tertiary care over the last five years in Türkiye was approximately 297 million.[12] Although blood pressure measurement is a basic and easily applicable method in hypertension screening, there are studies reporting that it is not performed regularly in health institutions. However, according to the PatenT2 study, it was found that blood pressure measurements were not performed at all for 15.5% of individuals who applied to healthcare institutions for any reason.[9] In a study conducted at a university hospital in Brazil, it was observed that blood pressure measurements were not conducted in two-thirds of outpatient visits.[13] Despite the recommendations for hypertension screening in many diagnosis and treatment guidelines and the widespread prevalence of hypertension in the community, the rate of blood pressure measurement is surprisingly low. The aim of this study is to evaluate the blood pressure measurement rates of patients presenting to different outpatient clinics.
Materials and Methods
Study design and ethical approval
This cross-sectional analytical study was conducted following approval from the Chief Physician of Farabi Hospital, Faculty of Medicine, Karadeniz Technical University (Approval No: 48814514-299), and the Scientific Research Ethics Committee of Karadeniz Technical University Faculty of Medicine (Approval No: 24237859-288).
Study population
The study population consisted of adults aged
18 years and older who applied to 24 different outpatient clinics of Karadeniz Technical
University Farabi Hospital between January 1, 2023, and January 1, 2024. These departments included: family medicine, dermatology, general internal medicine, endocrinology, gastroenterology, nephrology, hematology, medical oncology, immunology–rheumatology, cardiology, pulmonary diseases, infectious diseases, neurology, ophthalmology, physical therapy and rehabilitation, psychiatry, otolaryngology, orthopedics, obstetrics and gynecology, cardiovascular surgery, neurosurgery, general surgery, thoracic surgery, and plastic and reconstructive surgery.
Patients with incomplete medical history or physical examination notes were excluded. Additionally, the anesthesiology and urology departments were excluded due to the absence of patient documentation in the hospital information system. If a patient had multiple visits to the same clinic, only the most recent visit was included.
Data collection
Medical records were reviewed retrospectively via the hospital information system. Collected variables included age, sex, chronic disease status, medication use, and blood pressure (BP) measurement status during the patient’s last outpatient visit. For those whose BP was measured, values were recorded, and hypertension staging was performed based on the 2019 Turkish Hypertension Consensus Report: normal blood pressure was defined as systolic BP <120 mmHg and diastolic BP <80 mmHg; elevated blood pressure as systolic BP 120–129 mmHg and diastolic BP <80 mmHg; hypertension stage 1 as systolic BP ≥140 mmHg or diastolic BP ≥90 mmHg; and hypertension stage 2 as systolic BP ≥160 mmHg or diastolic BP ≥100 mmHg.[4]
Sample size calculation
Based on the findings of a previous pilot study reporting a 27.3% BP measurement rate[14], the minimum required sample size was calculated as 215 people for each branch outpatient clinic, 5160 people in total from 24 outpatient clinics, with a 90% confidence level, 5% margin of error, and a type I error of 0.05. The calculation was performed using OpenEpi Version 3. A total of 5160 patients—215 from each of the 24 outpatient clinics—were included in the study over a 12-month period.
Statistical analysis
Statistical analysis were conducted using IBM SPSS Statistics software. Numerical data were tested for normality using the Kolmogorov–Smirnov test. As the data did not follow a normal distribution, continuous variables were presented as median and interquartile range (IQR), while categorical variables were expressed as frequencies and percentages.
The Chi-square test or Fisher’s exact test was used for comparisons of categorical variables. Binary logistic regression analysis was performed to identify factors associated with BP measurement. Age, sex, presence of chronic disease, and hypertension diagnosis were included as independent variables, and the Enter method was applied. Odds ratios (OR) with 95% confidence intervals (CI) were reported. A p-value of less than 0.05 was considered statistically significant.
Results
Of the participants included in the study, 58.4% (n=3015) were female, with a median age of 48 (IQR: 32-62) years. 63.6% of the participants (n=3283) had at least one chronic disease. Those diagnosed with hypertension constituted 38.7% (n=1271) of participants with chronic diseases. 60% of participants (n=3097) were constant medication users. The characteristics of the participants are shown in Table 1.
| Table 1. Characteristics of the participants | |||
|
|
|
||
| Gender | Female |
|
|
| Male |
|
|
|
| Chronic Disease | Yes |
|
|
| No |
|
|
|
| Hypertension | Yes |
|
|
| No |
|
|
|
| Regular Medication Use | Yes |
|
|
| No |
|
|
|
It was observed that blood pressure was measured in 13.8% (n=712) of the participants during their outpatient examination. The median value for systolic blood pressure was found to be 120 mmHg (IQR: 110-140), and for diastolic blood pressure, it was 80 mmHg (IQR: 70-85). The departments with the highest rates of blood pressure measurement were nephrology (93%, n=200), cardiology (74.4%, n=160), general internal medicine (42.3%, n=91), endocrinology (39.5%, n=85), and family medicine (34.9%, n=75). No blood pressure measurements were found in any of the scanned patients in neurosurgery, dermatology, physical therapy and rehabilitation, ophthalmology, cardiovascular surgery, otolaryngology, oncology, orthopedics, plastic surgery, and psychiatry departments. The status of blood pressure measurement by specialty clinics is shown in Table 2.
| *Neurosurgery, dermatology, physical therapy and rehabilitation, ophthalmology, cardiovascular surgery, otolaryngology, oncology, orthopedics, plastic surgery, and psychiatry departments | |||||
| Table 2. Blood pressure measurement status by departments | |||||
| The last outpatient clinic visited |
|
|
|||
|
|
|
||||
|
|
|
|
|
||
| Nephrology |
|
|
|
|
|
| Cardiology |
|
|
|
|
|
| General Internal Medicine |
|
|
|
|
|
| Endocrinology |
|
|
|
|
|
| Family Medicine |
|
|
|
|
|
| Hematology |
|
|
|
|
|
| Neurology |
|
|
|
|
|
| Infectious Diseases |
|
|
|
|
|
| Immunology-Rheumatology |
|
|
|
|
|
| Thoracic Surgery |
|
|
|
|
|
| Pulmonary Diseases |
|
|
|
|
|
| Gastroenterology |
|
|
|
|
|
| General Surgery |
|
|
|
|
|
| Obstetrics and Gynecology |
|
|
|
|
|
| Others * |
|
|
|
|
|
| Total |
|
|
|
|
|
In the obstetrics and gynecology clinic, 44.7% (n=96) of the 215 patients were pregnant. Only 1% (n=1) of pregnant patients had their blood pressure measured. Among those whose blood pressure was measured, 49.7% (n=354) had a known diagnosis of hypertension. 11% (n=39) of patients diagnosed with hypertension had normal blood pressure based on the measurement results. Among those without a known diagnosis of hypertension, only 31.8% (n=114) had normal blood pressure measurements. When staging was performed based on the measurement results for individuals whose blood pressure was measured during their outpatient examination, 46.1% (n=328) had elevated blood pressure. The staging results based on blood pressure measurements are shown in Table 3.
| Table 3. Blood pressure staging based on measurement results | |||||||
|
|
|
|
|
|
|||
| Hypertension |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
| Total |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
||
Among all participants, 17.6% (n=577) of those with any known chronic disease and 27.9% (n=354) of those with known hypertension had their blood pressure measured during the examination (Table 4). In the nephrology clinic, 94.2% (n=129) of hypertensive patients had their blood pressure measured, 74.4% (n=93) in cardiology, and 73.9% (n=17) in family medicine, while no blood pressure measurements were recorded for hypertensive patients in some clinics. The status of blood pressure measurement among hypertensive patients by their last visited department is shown in Table 5.
| Table 4. Blood pressure measurement status according to the characteristics of the participants | |||||
| Total |
|
|
|||
|
|
|
||||
| Chronic Disease |
|
|
|
|
|
|
|
|
|
|
||
| Hypertension |
|
|
|
|
|
|
|
|
|
|
||
| Gender |
|
|
|
|
|
|
|
|
|
|
||
| Table 5. Blood pressure measurement status of hypertensive patients by departments | ||||
| Hypertension |
|
|
||
|
n (%) |
n (%) |
|||
| The Last Department Visited | Nephrology |
|
|
|
| Cardiology |
|
|
|
|
| Family Medicine |
|
|
|
|
| General Internal Medicine |
|
|
|
|
| Endocrinology |
|
|
|
|
| Hematology |
|
|
|
|
| Neurology |
|
|
|
|
| Infectious Diseases |
|
|
|
|
| Pulmonary Diseases |
|
|
|
|
| Neurosurgery |
|
|
|
|
| Dermatology |
|
|
|
|
| Physical Therapy & Rehabilitation |
|
|
|
|
| Gastroenterology |
|
|
|
|
| General Surgery |
|
|
|
|
| Thoracic Surgery |
|
|
|
|
| Ophthalmology |
|
|
|
|
| Immunology-Rheumatology |
|
|
|
|
| Obstetrics & Gynecology |
|
|
|
|
| Cardiovascular Surgery |
|
|
|
|
| Otolaryngology |
|
|
|
|
| Medical Oncology |
|
|
|
|
| Orthopedics |
|
|
|
|
| Plastic & Reconstructive Surgery |
|
|
|
|
| Psychiatry |
|
|
|
|
| Total |
|
|
|
|
In the family medicine clinic, 77.3% of individuals whose blood pressure was measured did not have a known diagnosis of hypertension. In the nephrology clinic, 64.5% of the measured patients had known hypertension, and in the cardiology clinic, 58.1% did (Figure 1).
As a result of logistic regression analysis, the factors associated with blood pressure measurement status were found to be the presence of a chronic disease (p<0.01), having a diagnosis of hypertension (p<0.01), and being male (p<0.01). Having a diagnosis of hypertension increased the likelihood of blood pressure measurement by 3.20 times (95% CI: 2.61-3.92), having a chronic disease by 1.64 times (95% CI: 1.30-2.08), and being male by 1.35 times (95% CI: 1.15-1.59). The odds ratios and confidence intervals for blood pressure measurement status according to variables are shown in Table 6.
| Table 6. Results of binary logistic regression analysis regarding factors that may affect blood pressure measurement status | |||
| Variables |
|
|
|
| Chronic Disease |
|
|
|
| Hypertension Diagnosis |
|
|
|
| Age |
|
|
|
| Gender |
|
|
|
Discussion
This study revealed that blood pressure (BP) was not measured in over three-quarters of outpatient visits. Despite the high burden of hypertension and its associated complications, this finding highlights a significant gap in routine clinical assessment. Departments with the highest measurement rates were nephrology, cardiology, and general internal medicine, while several clinics-including neurosurgery and oncology-recorded no BP measurements at all.
Approximately two-thirds of the participants had at least one chronic disease, and one-third had a known diagnosis of hypertension-similar to the 30.3% prevalence reported in the PatenT2 study.[9] However, only one-third of hypertensive patients in our sample had their BP measured. This pattern is consistent with earlier studies, which also reported low BP measurement rates in both primary care[15] and hospital settings.[13] These findings emphasize that BP monitoring is often overlooked, even in patients at high risk.
Among those measured, fewer than half had normal BP values, suggesting both undiagnosed hypertension and inadequate control in treated patients. In a study conducted in China, less than half of those diagnosed with hypertension were aware of their condition, and only 7.2% of patients receiving antihypertensive treatment had controlled blood pressure.[16] These figures highlight the global gap in hypertension diagnosis and management, supporting the need for routine BP checks during outpatient visits for both detection and follow-up.
Particularly concerning was the finding that only 1% of pregnant women in obstetrics and gynecology clinics had their BP measured, despite national data from the U.S. showing that hypertension contributes to approximately 7% of maternal deaths, with 70% of these occurring postpartum.[17] Similarly, in oncology clinics, the insufficient of BP screening is problematic given evidence that hypertension is the most common comorbidity among cancer patients (38%).[18] Furthermore, a large cohort study involving over 577.000 adults found that elevated mean blood pressure was associated with an increased risk of cancer in men[19], underscoring the importance of BP monitoring all specialties.
While nephrology, cardiology, and family medicine demonstrated relatively higher measurement rates, these remain insufficient. In departments with low or absent screening, such as general surgery and psychiatry, this likely reflects a limited focus on conditions perceived as outside the specialty scope. Additionally, time constraints and the absence of support personnel may further contribute to the omission of routine BP checks.
Our results also suggest that physicians are more likely to measure BP in patients with known chronic illnesses, especially hypertension and diabetes, possibly due to perceived risk. However, this selective approach limits early detection efforts. Notably, about three-quarters of those measured in family medicine clinics had no prior hypertension diagnosis, yet many showed elevated values-highlighting missed opportunities for intervention.
Given that effective BP control remains low in national and international studies[11,19], it is clear that routine measurement is essential not only for diagnosis but also for monitoring treatment response. The variability in BP measurement across departments may be attributed to inconsistent clinical habits, documentation gaps, or institutional workflow issues. Despite being conducted in a university hospital, where clinic personnel rotate frequently, the consistently low measurement rates point to systemic
shortcomings.
This study has several limitations that should be acknowledged. First, as a single-center study conducted in a university hospital, the findings may not be generalizable to other healthcare settings with different institutional structures, patient populations, or clinical workflows. Second, the retrospective design relied on outpatient examination records, which may not fully capture clinical practices. Blood pressure may have been measured during some visits but not documented, leading to potential underestimation of actual measurement rates.
Third, due to the educational nature of the institution, outpatient clinic staff rotate periodically. This variability in personnel may have influenced the consistency of clinical practices, including blood pressure measurement frequency. Fourth, the study did not include qualitative data to explore the reasons behind the omission of blood pressure checks in certain departments. Factors such as physician attitudes, perceived relevance, time constraints, or systemic barriers remain unclear.
Despite these limitations, the large sample size and inclusion of diverse outpatient departments provide important insights into current clinical practices and emphasize the need for improved routine hypertension screening.
Conclusion
Only 13.8% of outpatients had their blood pressure measured, highlighting a missed opportunity for early detection of conditions like hypertension. Given its potential complications, routine blood pressure assessment should be an integral part of all outpatient visits.
That fewer than half of those measured had normal results suggests both undiagnosed cases and suboptimal control among known patients. Physicians-especially in primary care-must prioritize regular measurement, supported by education, favorable working conditions, and manageable patient loads. Employing assistant health staff in clinics may also enhance adherence.
This and future large-scale studies can help raise clinical awareness of hypertension’s impact, identify gaps in current practice, and inform strategies to improve outcomes.
Ethical approval
This study has been approved by the Karadeniz Technical University Rectorate Faculty of Medicine Scientific Research Ethics Committee (approval date 09.05.2024, number 24237859-288). Written informed consent was obtained from the participants.
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39:3021-3104. https://doi.org/10.1093/eurheartj/ehy339
- Unger T, Borghi C, Charchar F, et al. 2020 International society of hypertension global hypertension practice guidelines. Hypertension. 2020;75:1334-1357. https://doi.org/10.1161/HYPERTENSIONAHA.120.15026
- Johnson KC, Whelton PK, Cushman WC, et al. Blood pressure measurement in SPRINT (Systolic Blood Pressure Intervention Trial). Hypertension. 2018;71:848-857. https://doi.org/10.1161/HYPERTENSIONAHA.117.10479
- Aydoğdu S, Güler K, Bayram F, et al. 2019 Turkish hypertension consensus report. Turk Kardiyol Dern Ars. 2019;47:535-546. https://doi.org/10.5543/tkda.2019.62565
- Beaney T, Schutte AE, Stergiou GS, et al. May measurement month 2019: the global blood pressure screening campaign of the international society of hypertension. Hypertension. 2020;76:333-341. https://doi.org/10.1161/HYPERTENSIONAHA.120.14874
- GBD 2017 Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392:1923-1994. https://doi.org/10.1016/S0140-6736(18)32225-6
- Türkiye İstatistik Kurumu (TÜİK). Death and causes of death statistics, 2022. Available at: https://data.tuik.gov.tr/Bulten/Index?p=Death-and-Causes-of-Death-Statistics-2022-49679 (Accessed on Jun 12, 2024).
- Chow CK, Teo KK, Rangarajan S, et al. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA. 2013;310:959-968. https://doi.org/10.1001/jama.2013.184182
- Sengul S, Akpolat T, Erdem Y, et al. Changes in hypertension prevalence, awareness, treatment, and control rates in Turkey from 2003 to 2012. J Hypertens. 2016;34:1208-17. https://doi.org/10.1097/HJH.0000000000000901
- Satman I, Omer B, Tutuncu Y, et al. Twelve-year trends in the prevalence and risk factors of diabetes and prediabetes in Turkish adults. Eur J Epidemiol. 2013;28:169-180. https://doi.org/10.1007/s10654-013-9771-5
- Oğuz A, Telci Çaklılı Ö, Tümerdem Çalık B, PURE Investigators. The Prospective Urban Rural Epidemiology (PURE) study: PURE Turkey. Turk Kardiyol Dern Ars. 2018;46:613-623. https://doi.org/10.5543/tkda.2018.32967
- Beştemir A, Aydın H. 300 million patient examinations per year; evaluation of emergency and polyclinic services of 2nd and 3rd stage public health facilities in Turkey. Sakarya Med J. 2022;12:496-502. https://doi.org/10.31832/smj.1128439
- Silva RP, Lima JW, Medeiros RP, et al. Blood pressure measurement in different outpatient clinics. Kidney Blood Press Res. 2010;33:235-239. https://doi.org/10.1159/000317101
- Özceylan ÖF, Set T. Polikliniklere başvuran hastaların kan basıncının ölçülme durumlarının değerlendirilmesi: bir kesitsel çalışma. 1. Karadeniz Aile Hekimliği Günleri, 2022 May 18, Samsun.
- Özceylan ÖF, Set T. Polikliniklere başvuran hastaların kan basıncının ölçülme durumlarının değerlendirilmesi: bir kesitsel çalışma. Farabi Tıp Derg. 2023;2:6-10. https://doi.org/10.59518/farabimedj.1295066
- Lu J, Lu Y, Wang X, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet. 2017;390:2549-2558. https://doi.org/10.1016/S0140-6736(17)32478-9
- Petersen EE, Davis NL, Goodman D, et al. Vital signs: pregnancy-related deaths, United States, 2011-2015, and strategies for prevention, 13 states, 2013-2017. MMWR Morb Mortal Wkly Rep. 2019;68:423-429. https://doi.org/10.15585/mmwr.mm6818e1
- Piccirillo JF, Tierney RM, Costas I, Grove L, Spitznagel EL. Prognostic importance of comorbidity in a hospital-based cancer registry. JAMA. 2004;291:2441-2447. https://doi.org/10.1001/jama.291.20.2441
- Stocks T, Van Hemelrijck M, Manjer J, et al. Blood pressure and risk of cancer incidence and mortality in the Metabolic Syndrome and Cancer Project. Hypertension. 2012;59:802-810. https://doi.org/10.1161/HYPERTENSIONAHA.111.189258
Copyright and license
Copyright © 2025 The Author(s). This is an open access article distributed under the Creative Commons Attribution License (CC BY), which permits unrestricted use, distribution, and reproduction in any medium or format, provided the original work is properly cited.