Öz
Objective: The aim of this study was to assess family physicians awareness of the concept of quaternary prevention and their attitudes towards defensive medicine.
Materials and Methods: The populations of this descriptive study were family medicine residents and family physicians working in primary care. The authors developed a “Quaternary Prevention Awareness Form” based on the literature. A questionnaire consisting of socio-demographic questions and the Defensive Medicine Practices Attitude Scale was administered online and face-to-face.
Results: The mean age of the 312 physicians was 39.22±9.55 years. Quaternary prevention had been heard of by 63.8% (n=199) of the physicians, but only 6.4% (n=20) had detailed knowledge of the concept. Although male physicians were more aware of “disease mongering” (p=0.003), females were more aware of “overtreatment” and “medical treatment management” (p=0.040; p=0.013, respectively). The results showed that males (p=0.007), residents (p=0.039) and those who had been sued for malpractice (p=0.004) had higher defensive medicine attitudes.
Conclusion: This study shows the importance of physicians’ awareness and knowledge, which have been enhanced by specialisation, urban practice and training in quaternary prevention. In order to protect society from the harms of excessive medical practices, medical education needs to be reviewed to remind us of “primum non nocere”.
Anahtar Kelimeler: family medicine, quaternary prevention, defensive medicine, awareness
Introduction
Family physicians are the first point of contact for patients within the healthcare system and provide a continuous healthcare service to the people under their care, from birth to death. This health service includes not only the treatment of illnesses that occur in people, but also the identification of risks and the protection of people against illness.[1]
In the last century, the increase in infectious diseases and the prolongation of human life have brought chronic diseases and the fight against them to the fore. This has highlighted the importance of preventive health services in the fight against these diseases, which require more comprehensive treatments and lifelong practices.[2] Leavell and Clark, who first contributed to the literature on prevention methods in the late 1940s, included the concepts of primary, secondary and tertiary prevention in their models of prevention.[3,4] The concept of quaternary prevention was first defined in 1986 by the Belgian general practitioner Marc Jamoulle and presented in 1995 as a new version of the “first do no harm” concept.[5-7] Although this model of prevention, which brings a critical perspective to the physicians’ own professional attitudes and practices and can vary according to person, time and situation, did not receive sufficient attention in the first years of its introduction, its importance and awareness are now gradually increasing. [4,6,8-12]
Defensive medicine, another important factor in quaternary prevention, is generally defined as deviation from standard medical practice due to fear of malpractice liability.[13] Deviation from medical practice can involve two types of behaviour: first, ordering more tests and procedures than medically indicated to reassure oneself and reduce the chance of missing something; second, avoiding high-risk procedures and/or patients because of malpractice liability.[14]
Awareness of quaternary prevention practices among family physicians, who are responsible for providing both preventive and curative health care, is extremely important for public health and efficient use of resources.[15] Unfortunately, there are not enough academic studies in the literature to assess the attitudes and awareness of family physicians on this issue. Therefore, the aim of this study was to determine the awareness of the concept of quaternary prevention and their attitudes towards defensive medicine practice among family physicians working in primary care, and to provide data for future studies on education and practice.
Materials and Methods
The universe of this descriptive and cross-sectional study consists of general practitioners and family physicians working in primary health care services. There were approximately 900 family physicians working in the region where the study was conducted during the specified date range. According to the sample calculation where the number of people in the universe is known, it was planned to include 269 physicians in the study with a 5% margin of error and 95% power. “The Quaternary Prevention Awareness Form, developed by the authors based on the literature, the Defensive Medicine Practices Attitude Scale and socio-demographic questions created a questionnaire form. It was distributed online to media groups of family physicians, residents and, if possible, face-to-face from 1 February to 31 May 2021. For the online questionnaire, the link to the survey was reminded a total of four times, two weeks apart. Approximately one-third of the data collected during the administration of the questionnaire was collected online, and the remaining two-thirds was collected face-to-face by visiting the physicians’ places of work. The questionnaire was left to the physicians, whose verbal consent was obtained by informing them prior to the questionnaire, to complete at their convenience, and the questionnaire was collected a few days later. The questionnaire took approximately 8-10 minutes to complete.
Exclusion criteria: The participant must be a native speaker of Turkish, as he/she must have a good command of Turkish to understand the scales and answer the questions, others were excluded.
The study was approved by the ethics committee of Necmettin Erbakan University Medical Faculty with the date 08.01.2021 and number 2021/3013.
Data collection instruments
The questionnaire used in the study consists of three parts: 1- Sociodemographic information form, 2- Quaternary prevention awareness form, which was inspired by previously published surveys on quaternary prevention and the literature on the subject, 3- Defensive Medicine Behaviour Scale (DMBS).[16]
1. Sociodemographic information form: It contains 18 descriptive questions such as age, sex, marital status, place of birth, level of academic education, time spent in the profession, institution of employment, satisfaction with professional career. There are also questions about education and knowledge of the concept of quaternary prevention.
2. Quaternary Prevention Awareness Form (QPA): This form, developed by the researchers, contains statements on quaternary prevention, which are examined under 11 subheadings in the literature.[8] These subheadings are 1. Information overload (1-4), 2. Overdiagnosis (5,6), 3. Medically unexplained symptoms (7-9), 4. Overmedicalisation (10,11), 5. Incidental findings (12,13), 6. Overscreening (14-19), 7. Overtreatment (20-27), 8. Shared decision-making (28-30), 9. Management of medical treatment (31-34), 10. Disease awareness (35,36) and 11. Evidence-based practice (37-42). These statements are answered as ‘strongly agree=5; agree=4; neutral=3; disagree=2; strongly disagree=1’. Some statements are reverse coded (8, 9, 13, 16, 20, 21, 22, 24, 25, 30, 40, 41, 42). An overall score for awareness of quaternary prevention and scores for the sub-headings were calculated. Higher scores on the quaternary prevention awareness form were scored as higher participant awareness of the quaternary prevention approach (Cronbach alpha=0.756).
3. Defensive Medicine Behavior Scale (DMBS): This scale, developed by Baser et al., has 18 statements in three subscales.[16] The first nine statements are designed to measure ‘attitudes towards positive defensive medicine practices’, the next five statements are designed to measure ‘attitudes towards negative defensive medicine practices’ and the last four statements are designed to measure knowledge about defensive medicine. The first two subscale statements have five-point Likert type responses, but the last part was prepared for ‘yes’ and ‘no’. In the reliability analysis, the internal consistency of the scale was found to be high (Cronbach alpha=0.853).[16]
Statistical analysis
The Statistical Package for Social Sciences (IBM SPSS) for Windows 26.0 was used for statistical analyses. Descriptive statistics for continuous variables were expressed as mean and standard deviation, while categorical data were expressed as frequencies and percentages. Normal distribution was tested by Kolmogorov-Smirnov. Independent samples t-test was used for paired groups and one-way analysis of variance (one-way ANOVA) for multiple groups to compare quantitative data. The difference between groups was assessed by post hoc Tukey test. A P value <0.05 was considered statistically significant. The relationship between variables was determined by Pearson correlation analysis. Correlation coefficient (r); 0.00-0.24 was considered as weak, 0.25-0.49 as moderate, 0.50-0.74 as strong, 0.75-1.00 as very strong relationship.
Results
The mean age of the 312 physicians was 39.22±9.55 (min: 23 max: 63) years. When the age of the participants was divided into three groups, 46.2% (n=144) were aged between 31 and 45 years. Of the participants, 53.8% (n=168) were female, 82.1% (n=256) were married, and 88.5% (n=276) lived in a nuclear family. Family medicine residents accounted for 33.7% (n=105) of all participants. 66.3% of participants (n=207) were actively practicing family medicine in a family health centre (FHC), 74.7% (n=233) were working in an urban area, and 48.4% (n=151) were satisfied with their career. They saw a median of 40 patients per day (min: 0, max: 100) and 43.9% (n=137) reported having enough time to spend with their patients. The concept of quaternary prevention was new to 36.2% (n=113) of the participants. Most (76.3%; n=238) had received no training in quaternary prevention and 67.9% (n=212) said they would like to receive training. The socio-demographic characteristics of the participants are shown in Table 1.
| Table 1. Sociodemographic characteristics of the participants | ||
| N=312 |
|
|
| Gender |
|
|
| Male |
|
|
| Female |
|
|
| Age (year) | ||
| 30 years and below |
|
|
| 31-45 years old |
|
|
| 46 years and older |
|
|
| Professional Position | ||
| Resident |
|
|
| Family Physician |
|
|
| Duration in the profession | ||
| 10 years and below |
|
|
| More than 10 years |
|
|
| Location of the Workplace | ||
| Urban area |
|
|
| Rural area |
|
|
| Patients cared for per day | ||
| 20 and below |
|
|
| 21-50 |
|
|
| Over 50 |
|
|
| Have you ever heard of the concept of “Quaternary Prevention”? | ||
| No, never heard of it |
|
|
| Yes, but I don't know the content of the concept |
|
|
| Yes, I have moderate knowledge |
|
|
| Yes, I have detailed information on the subject |
|
|
The internal consistency coefficient of the questionnaire was 0.726. The mean quaternary prevention awareness score of the participants was 149.74±11.15.
Family medicine residents had higher QPA scores (152.83±8.93) than general practitioners (148.16±11.83) (p<0.001). The QPA scores of family physicians working in urban areas (152.01±9.39) were also higher than those working in rural areas (143.02±13.14) (p<0.001). Physicians who had received detailed information about quaternary prevention (162.90±8.955) had higher QPA scores than those who had never heard about it (149.72±11.436) (p<0.001). The QPA scores of the participants according to socio-demographic data are shown in Table 2.
|
QPA: Quaternary Prevention Awareness DMBS: Defensive Medicine Behavior Scale One way ANOVA—Posthoc-Tukey test |
||||
| Table 2. Distribution of participants according to sociodemographic data in terms of DMBS and QPA scores | ||||
|
|
|
|||
| N=312 |
|
|
|
|
| Gender | ||||
| Male |
|
|
|
|
| Female |
|
|
||
| Age (year) | ||||
| 30 years and below |
|
|
|
|
| 31-45 years old |
|
|
||
| 46 years and older |
|
|
||
| Professional Position | ||||
| Resident |
|
|
|
|
| Family Physician |
|
|
||
| Duration in the profession | ||||
| 10 years and below |
|
|
|
|
| Over 10 years |
|
|
||
| Location of the Workplace | ||||
| Urban area |
|
|
|
|
| Rural area |
|
|
||
| Patients cared for per day | ||||
| 20 and below |
|
|
|
|
| 21-50 |
|
|
||
| Over 50 |
|
|
||
| Have you ever heard of the concept of “Quaternary Prevention”? | ||||
| No, never heard of ita |
|
|
|
|
| Yes, but I don't know the content of the conceptb |
|
|
||
| Yes, I have moderate knowledgec |
|
|
||
| Yes, I have detailed information on the subjectd |
|
|
||
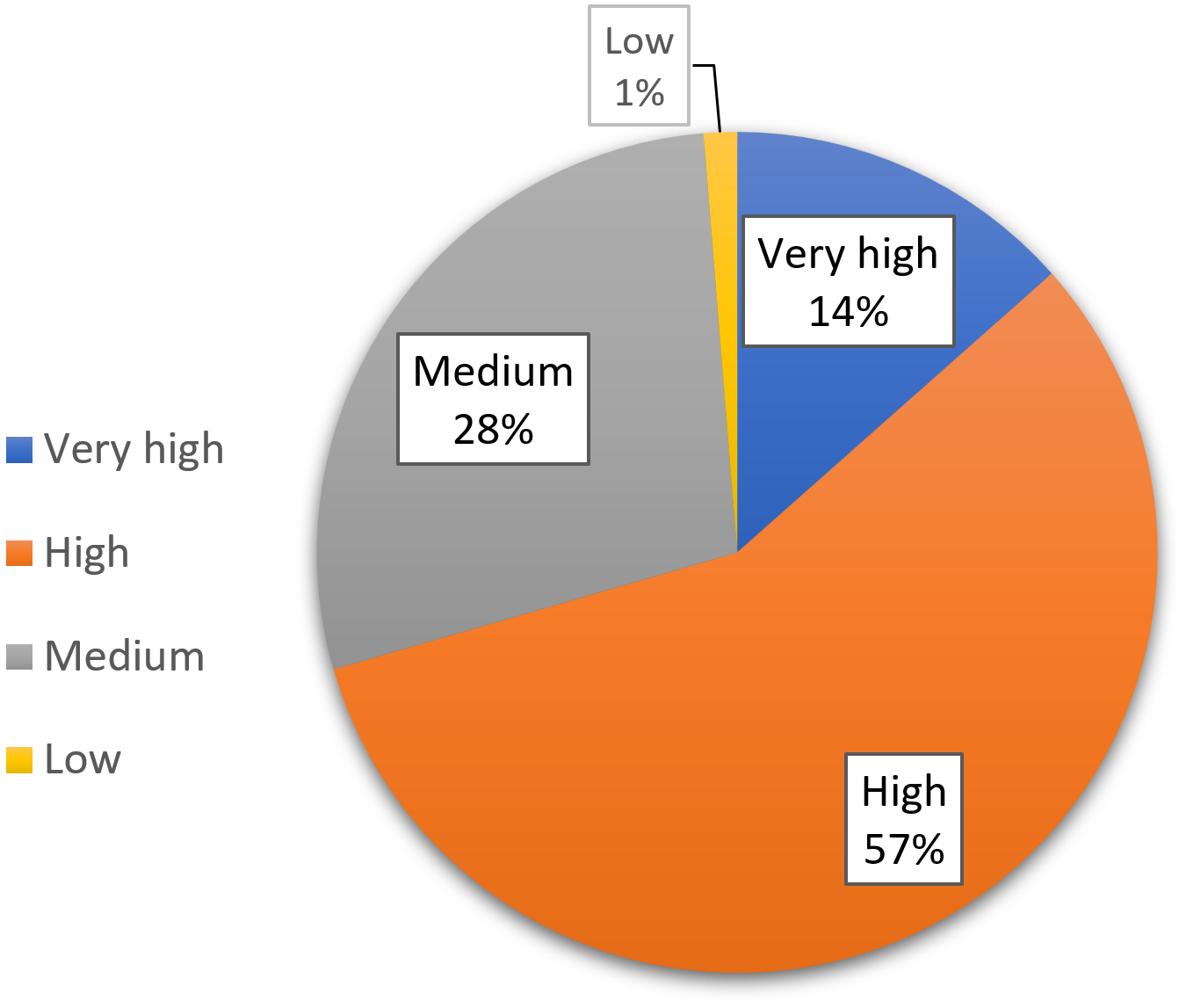
In the study, 9% (n=28) of physicians had experienced malpractice litigation during their medical career and 91% (n=284) believed that malpractice litigation had an impact on their medical performance. Although 71.2% (n=222) of physicians said they had heard of the concept of defensive medicine, 62.8% (n=196) said they did not know enough about it. The mean DMBS score of the participants was 45.86±8.63. Scale scores were categorised as very high (70-56), high (55-42), medium (41-28) and low (14-27). It was found that 70.6% (n=220) of the physicians in the study had very high (13.5%; n=42) and high (57.1%; n=178) levels of defensiveness. The internal consistency of the scale in this study was high (Cronbach’s alpha=0.830). The participants’ attitudes towards defensive medicine are shown in Figure 1.
The mean DMBS score of male physicians was significantly higher (47.28±9.11) than that of female physicians (44.64±8.03) (p=0.007). Participants aged 46 years and older had lower DMBS scores (45.14±8.51) than those aged 31-45 years (46.85±9.17) (p=0.036). Residents also had significantly higher DMBS scores (47.28±8.75) than general practitioners (45.14±8.51) (p=0.039). Those who had been sued for malpractice during their medical career had significantly higher DMBS scores (50.29±7.94) than those who had not (45.42±8.59) (p=0.004). Table 2 shows the mean DMBS scores of the participants according to socio-demographic data.
At the end of the socio-demographic form, participants were asked the open-ended question “What do you think are the reasons for unnecessary medical procedures? According to the participating physicians, the most common reasons for unnecessary medical procedures were patient will and coercion (25%), lack of knowledge and experience (16%), and fear of not being preferred by patients (13%).
The overinformation score of residents (17.61±1.66) was higher than that of general practitioners (16.53±2.27) (p<0.001). Those with less than 10 years’ experience had an overdiagnosis score of 7.84±1.24, while those with more than 10 years’ experience had a score of 7.50±1.49 (p=0.030). The overinformation (17.25±2.02) and overdiagnosis (7.77±1.37) scores of those working in urban areas were higher (p<0.001) than those living in rural areas (15.85±2.16) (7.29±1.43) (p=0.009). The scores of the participants according to their socio-demographic characteristics in the sub-dimensions of the QPA are shown in Table 3 and Table 4.
| *QPA: Quaternary Prevention Awareness **MUS: Medically unexplained symptoms. One way ANOVA—Posthoc-Tukey test. | ||||||
| Table 3. Evaluation of the participants' scores in the sub-dimensions of the QPA* according to their sociodemographic characteristics-1 | ||||||
| N=312 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Gender | ||||||
| Male |
|
|
|
|
|
|
| Female |
|
|
|
|
|
|
| p |
|
|
|
|
|
|
| Age (year) | ||||||
| 30 years and belowa |
|
|
|
|
|
|
| 31-45 years oldb |
|
|
|
|
|
|
| 46 years and olderc |
|
|
|
|
|
|
| p |
|
|
0.014ac |
|
|
0.013bc |
| Professional Position | ||||||
| Resident |
|
|
|
|
|
|
| Family Physician |
|
|
|
|
|
|
| p |
|
|
|
|
|
|
| Duration in the profession | ||||||
| 10 years and below |
|
|
|
|
|
|
| Over 10 years |
|
|
|
|
|
|
| p |
|
|
|
|
|
|
| Location of the Workplace | ||||||
| Urban area |
|
|
|
|
|
|
| Rural area |
|
|
|
|
|
|
| p |
|
|
|
|
|
|
| Have you ever heard of the concept of “Quaternary Prevention”? | ||||||
| No, never heard of itd |
|
|
|
|
|
|
| Yes, but I don't know the content of the concepte |
|
|
|
|
|
|
| Yes. I have moderate knowledgef |
|
|
|
|
|
|
| Yes, I have detailed information on the subjectg |
|
|
|
|
|
|
| p |
0.014df |
0.020ge 0.008df |
0.021ge |
0.035gd |
0.041 0.013 |
<0.001eg 0.017df |
| *EBMP: Evidence-Based Medical Practices. One way ANOVA—Posthoc-Tukey test. | |||||
| Table 4. Evaluation of the participants' scores in the sub-dimensions of the QPA* according to their sociodemographic characteristics-2 | |||||
| N=312 | Overtreatment | Shared decision-making | Management of medical treatment | Disease mongering | EBMP* |
|
|
|
|
|
|
|
| Gender | |||||
| Male | 26.55±3.50 | 10.06±1.47 | 15.35±2.23 | 8.18±1.40 | 20.44±2.89 |
| Female | 27.37±3.50 | 9.85±1.27 | 15.94±1.93 | 7.74±1.41 | 20.45±2.22 |
| p | 0.040 | 0.189 | 0.013 | 0.003 | 0.960 |
| Age (year) | |||||
| 30 years and belowa | 26.87±3.13 | 9.77±1.09 | 15.96±1.98 | 7.70±1.19 | 20.00±2.45 |
| 31-45 years oldb | 26.81±3.80 | 9.99±1.35 | 15.53±2.19 | 7.85±1.35 | 20.41±2.49 |
| 46 years and olderc | 27.30±3.36 | 10.03±1.57 | 15.63±2.04 | 8.31±1.19 | 20.88±2.67 |
| p | 0.576 | 0.404 | 0.348 | 0.006ac 0.019bc |
0.082 |
| Professional Position | |||||
| Resident | 27.33±3.27 | 10.10±1.13 | 16.13±1.69 | 8.07±1.12 | 20.88±2.15 |
| Family Physician | 26.826±3.63 | 9.86±1.46 | 15.43±2.24 | 7.88±1.36 | 20.23±2.71 |
| p | 0.230 | 0.112 | 0.002 | 0.236 | 0.022 |
| Duration in the profession | |||||
| 10 years and below | 26.92±3.45 | 9.90±1.19 | 15.92±2.06 | 7.72±1.24 | 20.41±2.58 |
| Over 10 years | 27.05±3.58 | 9.98±1.48 | 15.48±2.11 | 8.11±1.29 | 20.47±2.53 |
| p | 0.756 | 0.620 | 0.069 | 0.008 | 0.849 |
| Location of the Workplace | |||||
| Urban area | 27.47±3.21 | 10.13±1.23 | 15.99±1.79 | 8.11±1.21 | 20.72±2.22 |
| Rural area | 25.58±4.01 | 9.39±1.58 | 14.72±2.60 | 7.47±1.37 | 19.63±3.22 |
| p | <0.001 | <0.001 | <0.001 | <0.001 | 0.006 |
| Have you ever heard of the concept of “Quaternary Prevention”? | |||||
| No, never heard of itd | 27.17±3.47 | 10.03±1.485 | 15.58±2.03 | 8.14±1.40 | 20.58±2.64 |
| Yes, but I don't know the content of the concepte | 26.01±3.59 | 9.73±1.3 | 15.33±2.13 | 7.69±1.31 | 19.67±2.47 |
| Yes, I have moderate knowledgef | 27.15±2.80 | 9.91±1.20 | 15.91±2.18 | 7.88±1.09 | 20.76±2.37 |
| Yes, I have detailed information on the subjectg | 29.60±4.82 | 10.60±1.27 | 16.55±1.60 | 8.25±1.11 | 21.70±2.38 |
| p | 0.020gd <0.001gf 0.022fe |
0.063 | 0.063 | 0.060 | 0.020ge 0.006gd |
Discussion
The concept of quaternary prevention, which takes the model of preventive medicine to a new level, is a structure that is constantly being developed and renewed with the contributions of researchers and has an important place in the future of health care systems. The literature shows that there is a lack of studies on physicians’ attitudes towards the principles and approaches of quaternary prevention. With the present study, we aimed to contribute to the literature on quaternary prevention and to draw attention to the concept of quaternary prevention, which has not yet received sufficient attention in Türkiye. Because of its subject matter, because it is the first study on this topic, and because of its findings, this study makes important contributions to family medicine in particular. Quaternary prevention refers to a general medical approach. This approach includes attitudes and awareness of concepts such as overdiagnosis, overtreatment, management of medical treatment and stigma associated with quaternary prevention and patient-centred care. According to Jamoulle, person-centred care and the application of quaternary prevention are based on a construction between the perspectives, beliefs, values and experiences of patients and practitioners.[8-10]
For this purpose, subheadings related to quaternary prevention were identified in the questions asked of the participants and their opinions on these issues were asked. In this way, the study participants’ awareness of quaternary prevention can be examined from a broader perspective. This study found that the majority of doctors had heard of the concept of quaternary prevention, but very few had detailed knowledge of the subject. A study conducted in Peru found that almost all general practitioners were aware of quaternary prevention and that about two-thirds of them had very good knowledge of the subject. In addition, the majority of doctors who participated in the study emphasised that the concept of quaternary prevention was very important for the current health system.[17] It appears that awareness of quaternary prevention is low in Türkiye. Increasing physicians’ awareness of quaternary prevention through in-service training programmes and including it in the curriculum of medical schools will have positive outcomes for both physicians and the health system.
It has been suggested that overinformation can lead to overdiagnosis and overtreatment in two different ways. The first occurs as a result of the pressure that patients put on doctors due to misinformation they receive from environments where there is a lot of misleading information, such as the internet and social media.[18,19] Physicians under pressure from patients to test and treat may engage in off-label practices.[20-23]
The second situation arises from the increasing volume of scientific literature and the difficulty for physicians to keep up with the latest information. Physicians who are bombarded with information become confused about which medical procedures to perform. Physicians who find it difficult to choose the most appropriate medical procedures for the patient’s current condition may resort to unnecessary procedures rather than risk incomplete practice.[24] The study presented here explored patients’ attitudes to the situation created by the disinformation and misdirection to which they were exposed. The majority of physicians who took part in the study felt that over-information could lead to over-diagnosis and over-treatment.
If we look at the statements on exposure to excessive information, as well as other subgroup scores in the study, we see that residents, specialist family physicians, those working in urban areas, and physicians who have detailed information about quaternary prevention have better attitudes and awareness of the issue. The effect of physicians’ level of education on the differences in attitudes can be mentioned here. Physicians who have undergone or are undergoing specialist training would be expected to have a higher level of knowledge about newer concepts such as quaternary prevention and overinformation. Again, the fact that those with more detailed information about quaternary prevention are more aware of overinformation shows the importance of education on this topic. The reason for the difference between those working in urban and rural areas may be that physicians working in rural areas do not have a professional environment that encourages them to follow the latest scientific literature.
This study found that residents, those who had worked for 10 years or less, and those who worked in urban areas were more aware of overdiagnosis. Studies on the concept of overdiagnosis have increased in recent years and have attracted the attention of more and more physicians. For this reason, it is expected that the attitudes of physicians who have recently completed their medical training, and whose knowledge can be considered more up-to-date, would be high.
Participants under 30 years of age, general practitioners, those working in urban areas and those who had detailed information about quaternary prevention were more aware of ‘incidentalomas’. In a review of the literature, one study from the USA stands out, which examined the attitudes of patients and physicians on this issue. In the study, which focuses on overdiagnosis and overtreatment of low-risk thyroid cancer, physicians argue that thyroid imaging performed for unrelated reasons starts the cycle of overdiagnosis and overtreatment. It has been argued that nodules found incidentally on these imaging studies inevitably lead to overtreatment.[25] Incidentalomas sometimes lead to a reduction in mortality as a result of early diagnosis and treatment. However, many people who undergo detailed whole-body imaging may have suspicious findings.[26] Physicians should be sceptical that treating incidentalomas may do more harm than good to the patient. The higher scores for young physicians in this section may be related to their having a more questioning and critical perspective.
This study found that female participants, specialist family physicians, those working in urban areas and those who had detailed information about quaternary prevention had higher overtreatment scores. A study of physician attitudes to overtreatment found that the guidelines were more widely accepted than before, but that it was difficult to deviate from guideline recommendations in practice.[27] In a qualitative study conducted in Switzerland, physician anxiety, excessive caution and defensive attitudes towards overtreatment were attributed to physician factors, while time constraints and pressure from senior physicians were cited as examples of non-physician factors. It has also been suggested that lack of knowledge and clinical experience leads to overtreatment.[28] The literature suggests that as knowledge and experience increase, so does awareness of overtreatment. In line with these conclusions, the present study found that family physicians, who would be expected to have more clinical experience, had higher awareness of overtreatment. Although there was no difference between the sexes in the studies, the reason why female physicians had higher awareness in the present study may be the overriding idea of not causing harm as a result of establishing an empathic relationship with patients.
This study found that around three quarters of physicians had a highly defensive attitude to medical practice. The rate of physician defensiveness was found to be 75% in the United Kingdom[29], 93% in the United States[30], and 60% in Israel.[31] Again, studies have shown that the majority of physicians in Türkiye have defensive attitudes.[32,33] While defensive medicine practices increase the cost of health services, they also lead to patients being exposed to excessive medical procedures.[34] In order to prevent these situations, it is necessary to understand the reasons that lead physicians to adopt defensive attitudes and to take the necessary measures. In this study, physicians reported that the most common reasons for undertreatment were pressure and demands from patients, lack of knowledge and experience, fear of being disliked by patients, and defensive medicine. Similarly, in a US study, physicians reported that the most common reasons for overtreatment were fear of malpractice, pressure from patients, and difficulty in accessing past medical records.[35] A study of general practitioners concluded that fear of malpractice, clinical performance measures and lack of time led to overuse of medical services.[22] In another study in Germany, family physicians identified situations such as physicians’ lack of empathy and communication skills, low self-confidence due to lack of clinical experience, lack of preference for evidence-based medical guidelines, defensive medical practices, economic reasons and lack of a culture of discussion as leading physicians to overuse.[36]
Limitations of the study include the online administration of the questionnaire to participants due to the pandemic, the limited literature and the limited nature of the study. Because the study was conducted in a specific region, reached a limited number of participants, and used a survey method, the results cannot be generalised due to the possibility of individual bias, but may provide important guidance for future research groups. As there is no standardised scale in the study area, a questionnaire form developed by the researchers based on the literature was used. Future studies can develop a scale in this area and obtain more original results. Finally, the self-report design of the study may lead to bias.
Conclusion
The concept of quaternary prevention focuses on minimising the harm that can result from overuse of medical services. In this context, identifying the causes of overuse is of great importance for quaternary prevention. The concepts of overdiagnosis and overtreatment are not fully understood by most of society, including some physicians. Research is needed to identify medical practices that put people at risk of overdiagnosis and overtreatment and to take appropriate action. It is expected that public awareness will increase as the number of studies on the subject increases.
Ethical approval
This study has been approved by the Necmettin Erbakan University Non-Drug Medical Device Research Ethics Committee (approval date 08.01.2021, number 2021/3013). Written informed consent was obtained from the participants.
Source of funding
The authors declare the study received no funding.
Conflict of interest
The authors declare that there is no conflict of interest.
Referanslar
- Wonca Europe. The European definition of general practice/family medicine. Barcelona, Spain: WHO Europe Office; 2011. Available at: https://www.woncaeurope.org/file/27674b39-8f00-4577-b7d7-3fa912e93305/Definition%203rd%20ed%202011%20with%20revised%20wonca%20tree.pdf (Accessed on Sep 2, 2024).
- Basan NM, Bilir N. Prevention paradox and causes in preventive health services. TAF Prev Med Bull. 2016;15(1):44-50. https://doi.org/10.5455/pmb.1-1427871712
- Leavell HR, Clark EG. Preventive medicine for the doctor in his community: an epidemiologic approach. 3rd ed. New York: McGraw-Hill; 1960: 20-21.
- Pandve HT. Changing concept of disease prevention: from primordial to quaternary. Arch Med Health Sci, 2014;2(2):254-256 https://doi.org/10.4103/2321-4848.144366
- Jamoulle M. Information et informatisation en medecine generale. Belgique; 1986. Available at: https://orbi.uliege.be/handle/2268/170822 (Accessed on Sep 2, 2024).
- Jamoulle M, Roland M. Quaternary prevention. Available at: http://www.ph3c.org/PH3C/docs/27/000103/0000261.pdf (Accessed on Sep 3, 2024).
- Jamoulle M. Quaternary prevention: First, do not harm. MJ. P4 final draft. Available at: https://silo.tips/download/quaternary-prevention-first-do-not-harm (Accessed on Sep 3, 2024).
- Jamoulle M, Gavilán E, Cardoso RV, et al. The words of prevention, part II: ten terms in the realm of quaternary prevention. Rev Bras Med Fam Comunidade. 2015;10(35):1-11 https://doi.org/10.5712/rbmfc10(35)1063
- Jamoulle M. Quaternary prevention: First, do not harm. Rev Bras Med Fam Comunidade. 2015;10(35):1-3. https://doi.org/10.5712/rbmfc10(35)1064
- Jamoulle M. Quaternary prevention, an answer of family doctors to overmedicalization. Int J Health Policy Manag. 2015;4(2):61-64. https://doi.org/10.15171/ijhpm.2015.24
- Kuehlein T, Sghedoni D, Visentin G, Gérvas J, Jamoule M. Quaternary prevention: a task of the general practitioner. Available at: https://orbi.uliege.be/bitstream/2268/177926/1/2010-18-368_ELPS_engl.pdf (Accessed on Sep 4, 2024).
- Bae JM, Jamoulle M. Primary care physicians’ action plans for responding to results of screening tests based on the concept of quaternary prevention. J Prev Med Public Health. 2016;49(6):343-348. https://doi.org/10.3961/jpmph.16.059
- Annadurai K, Danasekaran R, Mani G, Ramasamy J. Quaternary prevention: preventing over-medicalization. J NTR Univ Health Sci. 2014;3(3):216-217. https://doi.org/10.4103/2277-8632.140955
- Assing Hvidt E, Lykkegaard J, Pedersen LB, Pedersen KM, Munck A, Andersen MK. How is defensive medicine understood and experienced in a primary care setting? A qualitative focus group study among Danish general practitioners. BMJ Open. 2017;7(12):e019851. https://doi.org/10.1136/bmjopen-2017-019851
- Tesser CD. Why is quaternary prevention important in prevention? Rev Saude Publica. 2017;51:116. https://doi.org/10.11606/S1518-8787.2017051000041
- Baser A, Baser Kolcu MI, Kolcu G, Gok Balcı U. Validity and reliability of the Turkish version of the defensive medicine behaviour scale: preliminary study. Anatol J Gen Med Res. 2014;24(2):99-102. https://doi.org/10.5222/terh.2014.29494
- Cuba Fuentes MS, Zegarra Zamalloa CO, Reichert S, Gill D. Attitudes, perceptions and awareness concerning quaternary prevention among family doctors working in the Social Security System, Peru: a cross-sectional descriptive study. Medwave. 2016;16(3):e6433. https://doi.org/10.5867/medwave.2016.03.6433
- Chen L, Wang X, Peng TQ. Nature and diffusion of gynecologic cancer-related misinformation on social media: analysis of tweets. J Med Internet Res. 2018;20(10):e11515. https://doi.org/10.2196/11515
- Sommariva S, Vamos C, Mantzarlis A, Đào LU-L, Martinez Tyson D. Spreading the (Fake) news: exploring health messages on social media and the implications for health professionals using a case study. Am J Health Educ. 2018;49(4):246-255. https://doi.org/10.1080/19325037.2018.1473178
- Jamoulle M. The four duties of family doctors: quaternary prevention-first, do no harm. Hong Kong Pract. 2014;36(2):72-77.
- Hill JA, following HEART Group Signatories , Agewall S, et al. Medical misinformation: vet the message!. Eur Heart J. 2019;40(5):404-405. https://doi.org/10.1093/eurheartj/ehz009
- Sirovich BE, Woloshin S, Schwartz LM. Too little? Too much? Primary care physicians’ views on US health care: a brief report. Arch Intern Med. 2011;171(17):1582-1585. https://doi.org/10.1001/archinternmed.2011.437
- Visentin G. The difficult choice of “not doing” comment on “quaternary prevention, an answer of family doctors to overmedicalization”. Int J Health Policy Manag. 2015;4(8):559-560. https://doi.org/10.15171/ijhpm.2015.108
- Wilson TD. Information overload: implications for healthcare services. Health Informatics J. 2001;7(2):112-117. https://doi.org/10.1177/146045820100700210
- Jensen CB, Saucke MC, Francis DO, Voils CI, Pitt SC. From overdiagnosis to overtreatment of low-risk thyroid cancer: a thematic analysis of attitudes and beliefs of endocrinologists, surgeons, and patients. Thyroid. 2020;30(5):696-703. https://doi.org/10.1089/thy.2019.0587
- Mariño MA. Incidentalomas: concept, relevance and challenges for medical practice. Rev Bras Med Fam Comunidade. 2015;10(35):1-9. https://doi.org/10.5712/rbmfc10(35)1053
- Ryskina KL, Holmboe ES, Bernabeo E, Werner RM, Shea JA, Long JA. US internists’ awareness and use of overtreatment guidelines: a national survey. Am J Manag Care. 2017;23(7):420-427.
- Eyer MM, Läng M, Aujesky D, Marschall J. Overtreatment of asymptomatic bacteriuria: a qualitative study. J Hosp Infect. 2016;93(3):297-303. https://doi.org/10.1016/j.jhin.2016.04.007
- Summerton N. Positive and negative factors in defensive medicine: a questionnaire study of general practitioners. BMJ. 1995;310(6971):27-29. https://doi.org/10.1136/bmj.310.6971.27
- Studdert DM, Mello MM, Sage WM, et al. Defensive medicine among high-risk specialist physicians in a volatile malpractice environment. JAMA. 2005;293(21):2609-2617. https://doi.org/10.1001/jama.293.21.2609
- Asher E, Greenberg-Dotan S, Halevy J, Glick S, Reuveni H. Defensive medicine in Israel - a nationwide survey. PLoS One. 2012;7(8):e42613. https://doi.org/10.1371/journal.pone.0042613
- Ozata M, Ozer K, Akkoca Y. Investigation of defensive medical applications of doctors who work in Konya city center. Gumushane University Journal of Health Sciences. 2018;7(1):132-139.
- Baser A, Kolcu G, Cıgırgil Y, Kadınkız B, Ongel K. Evaluation of the opinions of family doctors working in Izmir Karsiyaka district on defensive medical practices. Smyrna Med J. 2014;4(3):16-24.
- Berlin L. Medical errors, malpractice, and defensive medicine: an ill-fated triad. Diagnosis (Berl). 2017;4(3):133-139. https://doi.org/10.1515/dx-2017-0007
- Lyu H, Xu T, Brotman D, et al. Overtreatment in the United States. PLoS One. 2017;12(9):e0181970. https://doi.org/10.1371/journal.pone.0181970
- Alber K, Kuehlein T, Schedlbauer A, Schaffer S. Medical overuse and quaternary prevention in primary care - A qualitative study with general practitioners. BMC Fam Pract. 2017;18(1):99. https://doi.org/10.1186/s12875-017-0667-4
Telif hakkı ve lisans
Telif Hakkı © 2025 Yazar(lar). Açık erişimli bu makale, orijinal çalışmaya uygun şekilde atıfta bulunulması koşuluyla, herhangi bir ortamda veya formatta sınırsız kullanım, dağıtım ve çoğaltmaya izin veren Creative Commons Attribution License (CC BY) altında dağıtılmıştır.